Shellfish Allergy Symptoms and What to Do About It

Having a shellfish allergy is different from a fish allergy. Those who suffer from a shellfish allergy do not necessarily have to avoid eating fish and vice versa. It is important to avoid self-diagnosis and go to the emergency room to avoid severe flare-ups or anaphylactic shock.

Shellfish are generally marine and edible aquatic invertebrates with rigid exoskeletons. They come from 4 different families: Cephalops, Crustaceans, Gastropods and Echinoderms.
Table of Contents
Seafood and allergies.
However, in gastronomy we can differentiate two types of shellfish: crustaceans and mollusks. The most common edible crustaceans are:
- Shrimp.
- Crab.
- Prawn.
- Locust.
Mollusks include:
- Clams.
- Mussels.
- Oysters.
- Squid.
- Octopus.
- Snails.
- Scallops.
Of all food allergies, shellfish are responsible for 90% of cases. Crustaceans are more involved in severe allergic reactions than mollusks. It is by far the leading cause of allergy in adults.
It is seen more in adults than in children. In children, it is estimated that 0.1 to 0.9% of the child population has allergies to shellfish. Higher incidences have been reported with 4%.
- In Spain, it is responsible for 8% of allergies.
- In the USA more than 250,000 cases have been registered.
- Among the population of children and adolescents, the highest incidence is in males between 15 and 17 years of age.
- There are risk factors for sensitization:
Today it is known that exposure to shellfish is the most important environmental factor. Therefore, in places where shellfish are the usual diet, allergies are more frequent.
In the same way, the variety of shellfish involved depends on the most frequent local species in its gastronomy.
Risk factor’s.
There are individual risk factors, which can increase the symptoms and severity of the allergic reaction:
- Exercise or physical activity during or immediately after exposure.
- Acetylsalicylic acid intake.
- Regular use of beta-blockers, which is a type of medication for high blood pressure and some heart diseases.
- Intake of alcoholic beverages, because it increases intestinal permeability.
- Use of antiulcer drugs, which can alter the digestion of dietary proteins.
- Some immunosuppressants.
There are several proteins in shellfish involved in allergies. Those proteins or elements are called allergens. In the case of shellfish, they are water-soluble glycoproteins, the most common being tropomyosin, which is a muscle protein in shellfish, which also shows 87% similarity to other proteins: as in fruit flies, mites, helminths and some vertebrates. For this reason, sensitization can be done by contact with flies or mites and not necessarily by shellfish. There are cross allergies caused by tropomyosin.
Shellfish proteins are heat stable, meaning that they retain all their allergenic potential after cooking. Even allergens can be found in the cooking water or in the steam released by them.
There are two types of adverse reactions to food:
- Hypersensitivity or allergy.
Symptoms of allergic reactions to shellfish.
The symptoms are similar to other allergic reactions to food.
In general, allergic symptoms begin to appear between the first and third decade of life. Symptoms usually appear between 15 minutes and 120 minutes after contact with shellfish. However, late effects have been seen up to 7 hours later.
Atopic or allergic patients to other products tend to have more serious clinical varieties.
Skin manifestations.
Urticaria (rash) or angioedema, occurs in 28% of cases. It can be by direct contact on the skin or by ingesting the allergen.
Oral allergy syndrome.
Which is associated more with raw than cooked seafood, has 4 levels of severity
- Level 1: Oral manifestations, such as oropharyngeal pruritus or itching.
- Level 2: oral and gastrointestinal manifestations
- Level 3: oral symptoms associated with systemic or general symptoms: urticaria, angioedema, rhinoconjunctivitis and asthma.
- Level 4: Oral symptoms with life-threatening symptoms such as glottis edema and anaphylaxis.
It is the most frequent form when the allergen is only inhaled. Itching or itching in the throat and mouth are the mildest symptoms of shellfish allergies. It usually starts quickly after contact and subsides within 20 minutes. But in 70% of cases, it may be the first manifestation of a more severe presentation that occurs later.
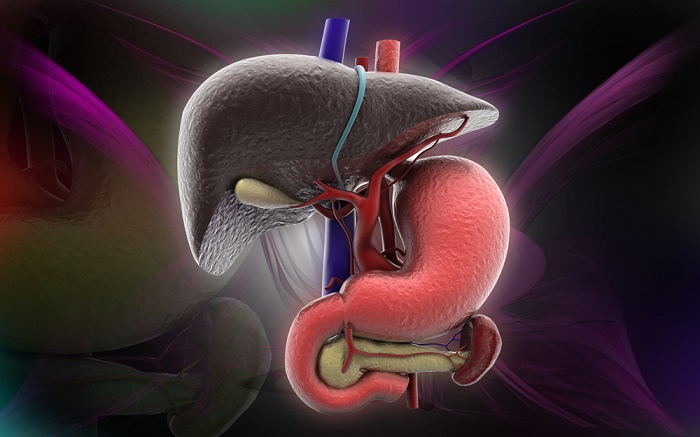
Gastrointestinal disorders.
Gastrointestinal manifestations are seen in 14% of cases. They start in minutes to 2 hours after ingestion of the allergen.
It is necessary to differentiate the symptoms of allergy with those of intoxication or those of infectious origin. They are very similar.
Respiratory problems.
Respiratory manifestations occur in 9% of cases and are more frequent in known atopic patients, with a history of bronchial asthma or with a family history of allergies. Respiratory symptoms are also seen more frequently with the ingestion of abalone, snails and limpets.
Anaphylaxis.
Anaphylaxis symptoms are seen in 7% of cases. They are severe symptoms with glottis edema and general collapse. It starts a few minutes after contact to hours.
The allergic manifestations shellfish can start with itching or pruritus, rash, angioedema (edema of the eyelids and lips), laryngeal edema, bronchospasm, abdominal cramping pain, diarrhea, hypotension, cardiovascular collapse and cardiac arrhythmia.
The clinical manifestations worsen with exercise after contact and combined with aspirin, antacid, alcohol and immunosuppressant intake.
Occupational disease caused by shellfish allergy.
It has been demonstrated that allergies to shellfish are greater in geographic areas and communities where shellfish is a frequent and common food in the diet.
It is not surprising that workers in the seafood industry have a higher incidence of allergic phenomena.
Shellfish proteins remain in the air during industrial production, as well as during cooking and handling.
They cause rhinoconjunctivitis in 18% of area workers. The risk factor is considered greater if there is a history of atopias and smoking.
What to do when you have shellfish allergies?
A good diagnosis should be established with: skin stimulation tests, laboratory tests with the determination of specific IgE antibodies.
- A shellfish-free diet is the best way to treat these allergies, including broths and avoiding kitchens or restaurants that handle a lot of shellfish.
- Always keep anti-allergy at hand.
- In severe cases, you can have a couple of doses of epinephrine auto-injectors.