Myofascial Pain Syndrome and fibromyalgia
Many of those who already suffer from fibromyalgia pain also suffer from myofascial pain syndrome. Syndrome myofascial pain is another form of chronic pain that can affect the entire body, including the face and jaw. Myofascial pain can add to the already bothersome symptoms of fibromyalgia, and can contribute to disability and a poor quality of life if not diagnosed correctly. If you think you may be suffering from myofascial dysfunction, consult with your healthcare provider to discuss your treatment options.
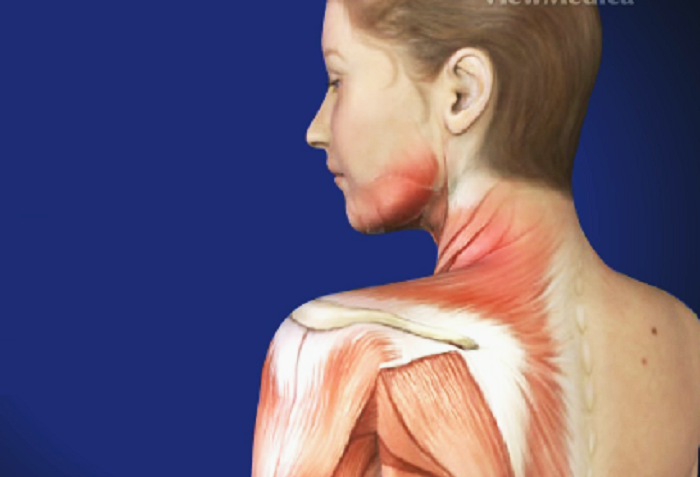
Table of Contents
What is Myofascial Pain Syndrome?
Myofascial syndrome is a pain disorder that affects muscles and fascia throughout the body. The fascia is like a network that surrounds the bones, tissues, organs, and blood vessels throughout the body. Myofascial pain syndrome can attack and cause degeneration of certain areas of the fascia, resulting in chronic pain and a variety of other symptoms.
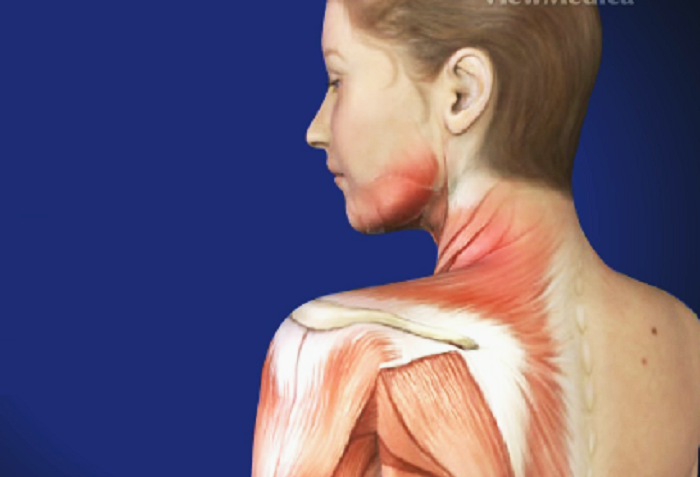
The pain usually originates in specific areas of the body, called myofascial trigger points (TrPs), which feel like tiny nodules under the skin. These trigger points commonly develop throughout the body, usually where the fascia comes into contact with a muscle.
Myofascial pain syndrome is a very common disease, and most people will develop at least one trigger point in their body at some point in their lives. Most of these people will not develop severe symptoms and will be able to continue with their normal routines. However, about 14% of the population will develop a chronic form of the syndrome, resulting in persistent pain and discomfort.
Myofascial pain disorder is very common in fibromyalgia patients. Myofascial pain syndrome was thought to be actually a kind of fibromyalgia. However, this is now known to be not the case. It is possible to have fibromyalgia and chronic myofascial syndrome, and therefore it is important to be diligent in analyzing your symptoms. If you notice symptoms of myofascial syndrome, write them down and report them to your doctor.
Signs and Symptoms of Myofascial Pain Syndrome.
The most common sign of myofascial pain is the presence of palpable trigger points in the muscles. Trigger points are areas of extreme sensitivity, and they usually form in bands of muscle under the skin. They are similar to tender points caused by fibromyalgia, only that trigger points can be felt under the skin.
When touched, the trigger points will cause pain and spasms in the muscles. Often the pain is felt in an area other than the trigger point that is actually affected, this is called referred pain.
Myofascial pain is usually a dull ache, but it can also produce a throbbing, stabbing, or burning sensation. The pain is often localized in the jaw area, although any part of the body can be affected. One-third of those with myofascial pain report localized pain, while two-thirds report pain all over their body.
Myofascial pain can also produce a variety of other symptoms, many of which may seem unrelated. These include:
- Numbness in the limbs.
- Popping of the joints.
- Limited movement of the joints, particularly the jaw.
- Muscle weakness (manifested in dropping things).
- Migraine or headache.
- Disturbed dream.
- Balance problems.
- Tinnitus and earache.
- Double vision or blurred vision.
- Memory problems.
- Unexplained nausea, dizziness, and sweating.
Aggravating factors.
Symptoms are usually aggravated by specific factors. Stress and anxiety contribute to muscle tension and can irritate trigger points. Changes in the weather, including sudden coldness, high humidity, or extreme dryness can also exacerbate symptoms. Physical activity can also trigger symptoms.
Causes of myofascial pain syndrome.
There are numerous causes of myofascial pain.
Muscle and skeletal problems.
The causes of myofascial pain dysfunction syndrome can be numerous and depend on the individual. Generally, myofascial pain is caused by some type of trauma to the muscles and skeleton in the body. Overworking the muscles can cause damage to certain areas leading to the development of a trigger point.
Poor posture can also trigger myofascial pain in certain individuals. Skeletal abnormalities, such as having different sized feet, fingers, or legs, can also contribute to the development of myofascial pain. Frequent exposure to cold weather can also increase the risk of developing chronic myofascial pain syndrome.
Chronic Fibromyalgia Pain.
People with fibromyalgia can have myofascial pain syndrome as a result of their fibromyalgia pain. Compensating for pain can often cause reduced movement or unhealthy posture, leading to the formation of trigger points.
The severe pain caused by fibromyalgia also causes muscle contractions around soft spots. Eventually, these muscle contractions cause trigger points to form, in addition to the fibromyalgia soft spots.
Depression associated with fibromyalgia.
Depression associated with fibromyalgia can also cause myofascial pain to develop. At least 30% of fibromyalgia patients suffer from depression, which causes low levels of serotonin in the brain. Serotonin is a neurotransmitter responsible for regulating mood and pain in the body. Depression can interfere with the process of regulating pain, causing SDM.
Effects of SDM on fibromyalgia.
Having both myofascial pain syndrome and fibromyalgia can be quite upsetting at times. The symptoms of myofascial pain and fibromyalgia are very similar, making it difficult for medical professionals to correctly diagnose many people.
Without a proper diagnosis, a patient may not receive proper treatment making the symptoms even worse. Additionally, myofascial pain can often contribute to fibromyalgia pain, making life much more difficult to enjoy.
Overmedication in traditional medicine.
Antidepressants and anti-anxiety medications are two of the most common medications prescribed for chronic pain, in the US alone with more than 250,000,000 prescriptions written each year, and growing. Therefore, it is not surprising that they are also part of the treatment protocol for myofascial pain syndrome and others.
One drug that is gaining popularity in recent days in the treatment of chronic pain syndromes is methadone. Methadone has been reported to be up to 20 times stronger than Vicodin or Percocet, which also makes methadone a much more dangerous drug.
Tizanidine (car flex), is another commonly prescribed medication for nerve pain. One of its most dangerous side effects is liver toxicity, along with potential drug interactions.
The most common advice doctors offer to these patients is simply learning to live with their respective syndromes along with pain management (medications). And many doctors who don’t offer much hope for pain relief often even advise against holistic options like chiropractic, acupuncture, nutritional treatments, and others that don’t bring any side effects.
Nutritional deficiencies related to myofascial pain.
Pain syndromes such as:
- Fibromyalgia.
- Myofascial pain syndrome (chronic myofascial pain).
- Chronic Fatigue Syndrome.
- Restless leg syndrome.
They all have studies linking these conditions to nutritional deficiencies. And there are three nutrients that stand out for being deficient in people with chronic pain: they are magnesium, vitamin D, and vitamin B12.
Natural treatments to relieve myofascial pain.
While contemporary medicine suggests special medications for myofascial pain, there is a wide range of home remedies and natural treatment options that one can benefit from.
Remember that first of all it is to look for alternatives to stay stress-free and keep your mind occupied in another place that is not the pain that is what reaffirms you that you suffer from it and there is an endless feedback loop.
-Vitamin D deficiency or hypothyroidism are often linked with this condition, therefore, treating these deficiencies is an important part of the treatment regimen. Get adequate exposure to the morning sun, to help the body synthesize its own vitamin D. Vitamin D supplements can also be beneficial in managing the condition. Make sure your diet is rich in iodine.
– Physiotherapy that includes a simple stretching, muscle strengthening and posture exercises, can be very beneficial.
– Massaging the body with aromatherapy essential oils such as cloves and lavender are considered very useful. Massage helps calm cramps and spasms and loosen tight muscles.
– Homeopathy has a profound benefit in the management of myofascial pain. The homeopathic drugs namely Rutha and Rhus Tux are very effective when taken in low doses and repeated several times a day.
– Look for therapies that keep you happy, in a good mood and producing hormones of happiness such as oxytocin and endorphins. Seek to set aside an hour a day by practicing walks, dancing, singing, doing creative therapy too that keeps you busy and doing what you love to do every day. Don’t forget that the mind is where most of the things that your body reflects happens.
Acupuncture is an alternative method of treatment for myofascial pain helping to relieve symptoms naturally. It can also provide some relief from the negative side effects of medications already used by the patient.
– Magnesium is a mineral that our body needs to carry out more than 300 biochemical reactions. It is the support that makes our muscles and nerves work normally, in addition, it helps to maintain a constant heart rate, keeps our bone structure strong and the immune system as well. Take a tablespoon of liquid magnesium in the morning and at night before going to bed.
– Make sure you take an adequate dose of vitamin D as this vitamin is essential to keep teeth and bones in optimal condition because it contributes to the absorption of calcium and phosphorus, which are key minerals for bone health. A vitamin D deficiency could cause osteoporosis and a malfunction of the nervous and muscular systems, therefore.
– Use iodized salt and increase the intake of shellfish such as shrimp, fish, seaweed, etc.
– Make sure your diet is rich in fresh fruits, fresh vegetables, Omega 3 essential fats. Avoid processed and refined foods. Reduce your alcohol intake, as it can lead to myofascial pain.


